A Whole River approach to the mental health care crisis
Health systems can maximize their impact on mental health disparities through a strategic asset alignment strategy.
This article discusses mental health and suicide ideation. If you or a friend need urgent assistance, call 911 immediately, or take your friend directly to the emergency room. If you feel it’s safe, stay with your friend, or find someone to stay with them until help arrives. You can also reach free, confidential support via the National Suicide Prevention Lifeline by dialing 988 24/7.
For years, the rate of mental illness among adults in the United States has been a stubborn statistic, plateauing at approximately 1 in 5 adults having a mental health condition by most studies and surveys. More alarmingly, the rate of children and young adults experiencing mental illness and mental health concerns has increased significantly over the past several years, accelerated by the COVID-19 pandemic and other societal phenomena. Today, suicide is the 2nd leading cause of death among children ages 10-14. As with most health conditions, there are significant disparities in diagnosis and treatment among Black, Indigenous, Pacific Islander, Alaskan Native, Hispanic and multi-racial Americans, as well as for those who identify as LGBTQIA+.
Not only do mental health inequities cost the United States a significant amount in direct and indirect costs, they are also driving approximately $23.9 billion in excess costs associated with already expensive chronic conditions like diabetes, hypertension, and HIV/AIDS and $5.3 billion in excess costs associated with emergency department visits. And while there are approved and effective treatments for most mental health conditions, the majority of adults (57%) and youth (60%) experiencing symptoms of a mental illness do not receive treatment.
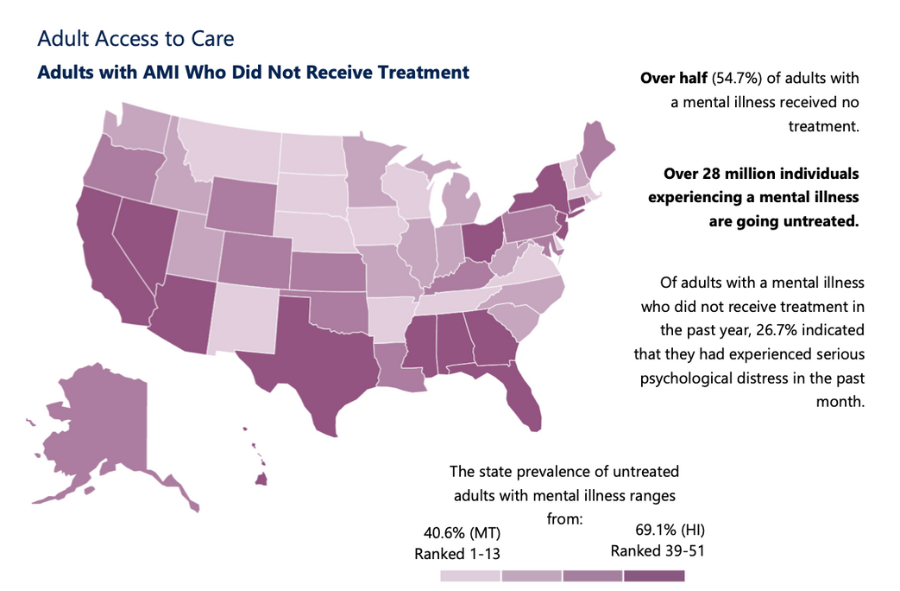
Mental Health America’s 2023 “State of Mental Health in America” report
The causes of disparities in mental health diagnosis, treatment and impact are numerous and complex but there are several clear drivers that health systems are uniquely positioned to impact, particularly in terms of increasing access to services. Health systems and other health impact investors can have an immense impact on this facet of the mental health crisis with a Whole River Paradigm approach to asset alignment.
Access to Services
A lack of mental health providers across the country– particularly in rural areas– is a major aspect of why so few people with mental illnesses receive treatment. On average, there are 350 people for every 1 licensed mental health provider and 37% of the U.S. population lives in an area with a severe mental health provider shortage. A recent analysis concluded that more than 6,000 additional mental health professionals are needed to fill the provider gap.
Increasing the workforce pipeline: Many health systems have already invested in programs to increase the nursing workforce and expand clinical career opportunities to historically disinvested communities. In particular, investment to increase the diversity of the mental health workforce– in terms of race, ethnicity, language, and geography– is paramount. Health investors should consider expanding this focus to invest in the mental health provider pipeline through scholarships, low- or no-interest student loans, and career impact bonds, a model introduced by Social Finance in 2019.
Supporting community-based services: The types of entities that provide mental health services expands beyond traditional clinical practices and can be expanded through more financing. One innovative example is Humana’s investment in a Substance Use Disorder (SUD) treatment and recovery program for pregnant women and their families in Louisville, Kentucky operated by Volunteers of America, a national non-profit with local affiliates. With Humana’s initial funding, VOA was able to design and scale their program and then secure contracts with other health plans in the area to cover the services costs for their members. Health systems and foundations with grantmaking portfolios can also make meaningful contributions to community-based organizations, like Interface Children & Family Services and Project Lift, that deliver therapeutic services to often underserved populations.
Expanding telehealth: While there is some debate about the efficacy of certain telehealth models, several promising studies indicate that phone and video mental health counseling can be an effective treatment model that increases access to services for millions of people. Health systems can invest in these services in a variety of ways including making equity investments in companies that are facilitating teletherapy services and increasing access to high-speed internet. Health systems can also be powerful advocates for public policy changes that enable health plans to cover remote therapy services beyond COVID-19 era exceptions and to increase government-funded subsidies for internet access.
Affordability
The most prevalent reason adults report not receiving mental health treatment is cost. Even individuals who have health insurance find it difficult to find and afford treatment for the duration necessary to see improvement in mental health symptoms. The affordability of mental health services can be addressed from multiple angles including the cost of services themselves, the opportunity cost individuals bear of seeking services, and sufficient individual and household financial resources to pay for services.
Mental Health America, 2023
Reduced-cost services: As clinical care providers, health systems should assess availability of reduced-cost mental health services in their communities and identify ways to offer sliding-scale or discounted rates to patients experiencing financial strain. Other strategies, like implementing group therapy programs, can help increase availability of affordable treatment for more people.
Insurance coverage: While mental health services can still be prohibitively costly with health insurance, uninsured individuals are even less likely to seek medical care than their insured counterparts. Health systems can partner with or invest in community-based organizations and social-impact companies working to increase enrollment in Medicaid and other insurance plans. One recent example is UPMC’s partnership with Fabric Health to enroll Pittsburgh residents who were disenrolled from Medicaid after COVID-19 exceptions expired.
Purchasing power: Ultimately, an individual or household’s ability and willingness to seek mental health services may depend on their financial resources. With 48% of Americans recently reporting that they have no money left over after paying their expenses each month, and 1 in 8 unable to afford an unexpected $400 emergency, the number of people without the funds to pay for care is enormous. Health systems committed to an @Healthcare Anchor Network strategy can prioritize economic development and financial mobility through local hiring and procurement practices and investing in the local infrastructure that helps lift people out of poverty. Health systems like Boston Medical Center are also funding or directly implementing evidence-based services like financial coaching to help patients manage and pursue improved credit scores, savings behaviors, and debt reduction. Keeping in mind that health system employees may themselves live with or care for someone who lives with a mental health condition, ensuring that employees have access to high quality health insurance, mental health treatment services, and a living wage should also be part of a holistic strategy to address mental health disparities.
Stigma and Knowledge
Over the past three decades, there has been significant investment and collaboration in campaigns and initiatives to reduce the stigma associated with mental illness, suicide, and helpseeking. Numerous public figures, including professional athletes, politicians and celebrities, have been publicly open about their own experiences with mental health and suicide, catalyzing a much more open dialogue about these topics than in previous decades. Still, stigma remains a prominent barrier to mental health treatment for many.
Public Awareness and Education: Health systems have a wide range of assets they can leverage to continue destigmatizing mental illness. Marketing campaigns and collateral that promote help-seeking and mental health services (like Nationwide Children’s campaign around childhood mental health), encouraging staff to volunteer as speakers and educators at schools, and sponsoring and providing information and resources at community events are all great ways for health systems to contribute to open, positive narrative change around mental health.
Open Conversations: Leaders and care providers across sectors can also play a major role in reducing stigma by being open about their own mental health experiences, especially given the high rates of depression and suicide ideation among healthcare workers. For example, Dr. Anne Pendo, who leads provider experience and wellbeing at Intermountain Healthcare, has regularly shared about her own experience losing a son to suicide and insights from her work supporting mental health among clinical providers. And Shawn Lesser, former co-founder and managing director of Big Path Capital, founded The Real Mental Health Foundation based on his own experience with anxiety.
Research: Despite extensive research to better understand the prevalence, causes, and effective treatments of mental health disorders, much is still unknown. In particular, there is limited research that centers non-white, non-cisgender, non-heterosexual people nor is there significant research about the mental health impacts– and potentially effective interventions– of intersectional issues like racism, financial strain, incarceration, and nutrition insecurity. As institutions with significant research capabilities and resources, health systems could create dedicated research portfolios or grant programs to support research that advances our understanding of how to better identify and treat mental health conditions across diverse populations and circumstances. As an initial step, researchers should consider adding a mental health metric that can be tracked to studies they plan to conduct.
Aligned Impact Funds
The demand for innovation in solutions addressing mental health has spurred new social enterprises and venture funds. For example, What If Ventures is a venture capital fund that supports and invests in companies addressing stigmatized healthcare problems. Philanthropic funds like Hopelab, with funding from the Omidyar Network, align and seed innovations in mental health solutions. InStride Health, a startup providing affordable specialty outpatient care for youth, has raised more than $50 million from health-focused investors including a recent $30 million raise that raised capital from Hopelab alongside General Catalyst and Mass General Brigham Ventures.
In fact, health systems with venture portfolios, like Mass General Brigham Ventures and Kaiser Permanente Ventures, align their strategies with their mission to invest in innovations supporting mental health. Furthering the impact of their partnership, Humana and VOA also created the Futures Fund, a social impact investment fund that supports the development and expansion of high impact health, housing and social service models within the VOA network.
What’s next?
Rising rates of mental illness and suicide ideation have spurred demand for capital and innovative solutions from investors and funders. Entrepreneurs, social justice advocates, non-profit organizations, government agencies, and healthcare providers are all important market players we’ll need engaged to combat this crisis. Health systems, in particular, are well positioned to make an enormous impact on the various factors driving disparities in access to quality care and treatment. We are heartened to see more investment across the board, and look forward to helping health impact investors align their assets to maximize impact.